In This Post:
Presenters:

Nataly Youssef
CEO and Founder

Scott Fillenworth
Chief Revenue Officer
Healthcare affordability is a significant issue in America. Across the country, too many people defer or skip needed healthcare services because they cannot pay for them. The fact that matters is that financial resources are available to both employees and employers. They’re just hidden behind complexity, confusion, and missed opportunities.
45% of Americans receive erroneous health care bills every year, and the majority of those are not in a member’s favor. Almost 50% of employees lose FSA dollars annually because no one shows them how to make the most of them and utilize those funds over the year. And voluntary benefits? We all know that there is a problem with voluntary benefits payouts with loss ratios at such low levels.
Reclaim Health exists to unlock the full financial value of healthcare benefits so people can stop worrying about what care costs and start focusing on getting the care they need. Because when people understand their benefits, when billing is accurate, and when dollars are working smarter, everyone wins. That was the heart of our latest webinar. Nataly Youssef, CEO and Founder at Reclaim Health, and Scott Fillenworth, Chief Revenue Officer at Reclaim Health, shared how Reclaim is reimagining what’s possible, using AI-powered insights and real human guidance to turn confusion into clarity and complexity into confidence. It’s a new kind of healthcare experience, one that empowers people, delivers real savings, and brings care within reach.
About Reclaim Health
Reclaim Health’s mission is simple: help employees and employers get the most out of their healthcare dollars and optimize the financial value of healthcare benefits. In an era where rising healthcare costs are increasingly unsustainable, both sides are seeking smarter ways to stretch every healthcare dollar.
Reclaim’s solution applies AI-powered insights and human advocacy to proactively detect billing errors, recover funds, and maximize the value of every benefit available. With over 1.5 million families and 100+ employers relying on Reclaim, the platform transforms how organizations approach healthcare affordability and efficiency.
Reclaiming healthcare dollars
According to recent studies, 74% of families struggle to afford healthcare:
- 45% of people forfeit Flexible Spending Account (FSA) funds because no one shows them how to make the most of this benefit.
- 47% receive erroneous health care bills every year.
- 90% miss filing for eligible voluntary benefits simply because the system is too complex.
Despite employers investing heavily in benefits packages, a significant portion of the financial value goes unrealized. Employees lack the support to understand and access their full range of benefits, leading to missed opportunities and reduced employee satisfaction.
Reclaim Health bridges this gap by integrating advanced AI with human expertise going far beyond traditional benefits administration by proactively monitoring claims, detecting inaccuracies, and advocating for payment corrections and reimbursements without any action required from employees.

Payment Advocacy in Action – Reclaim’s AI and human advocates work in tandem to:
- Identify billing errors (e.g., double billing or upcoding)
- Pause bill collection and initiate provider reviews
- Resubmit claims for corrected processing
- Secure reimbursements and credits for employers and employees alike
One real-life example of when healthcare service was incorrectly billed, leading to double charges. Reclaim detected the error, intervened, and saved the employee $1,000 and the employer $4,000.
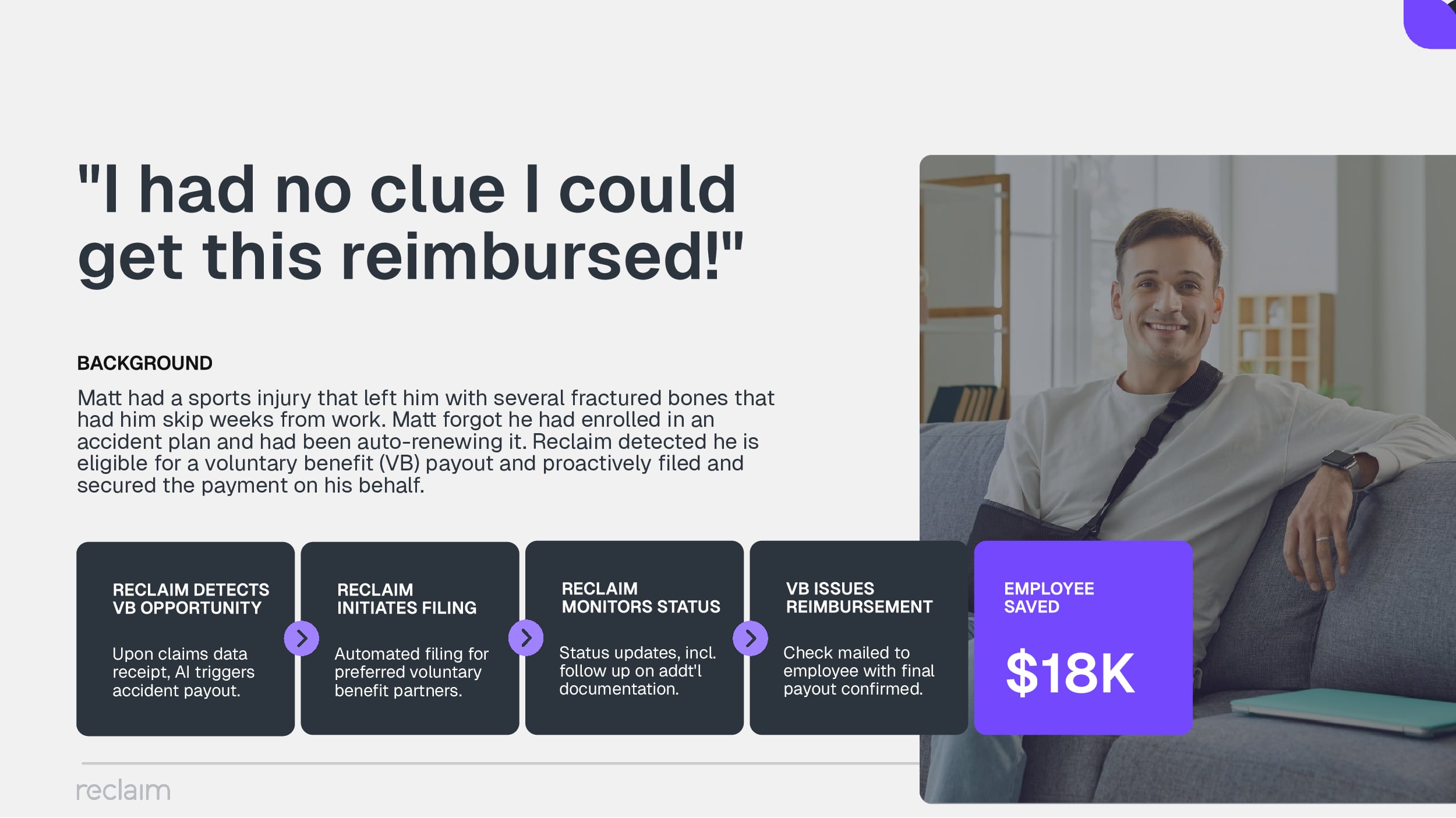
Another story involved a member who had a sports injury and forgot he had an accident plan. Reclaim detected his eligibility for a payout and initiated the claim automatically, securing $18,000 on his behalf.
Optimized Benefits Through AI Insights – By analyzing comprehensive line-by-line medical and pharmacy claims data, Reclaim recommends benefit plan changes, pre-tax contribution adjustments, and opportunities for voluntary benefit reimbursements. This helps:
- Prevent overspending on underutilized plans
- Maximize HSA/FSA usage
- Ensure better fit between benefits and employee needs
Year-Round Savings and Engagement – Unlike one-time audits, Reclaim operates continuously—24/7/365—monitoring all claims and identifying savings opportunities as they arise. It is:
- Seamlessly embedded in benefit ecosystems
- Fully portable across different vendors
- Automatically enrolled for most employees during open enrollment
- Zero-touch for employees, yet yields significant impact
This automated system ensures that both employers and employees benefit from real dollars reclaimed, year after year.
Analytics and Reporting for Transparent Impact
Reclaim also helps employers understand where their healthcare budget is going and how to improve it. Real-time dashboards and analytics provide insights into:
- Claim error trends
- Engagement with voluntary and medical benefits
- Forecasts for future benefit optimization
Employers receive visibility into program adoption, financial impact, and opportunities for better benefit utilization.
Optimizing every dollar your healthcare benefits have to offer
On average, Reclaim returns $6.3 million per 10,000 covered families, equating to approximately 3.5% of total medical spend. This financial relief goes directly back into employer budgets and employee pockets.
Savings are realized from::
- Billing Corrections
- Reimbursed Voluntary Benefits
- HSA/FSA Tax Benefits
- Medicare Transitions & Coverage Adjustments
Get in touch with Reclaim Health today!
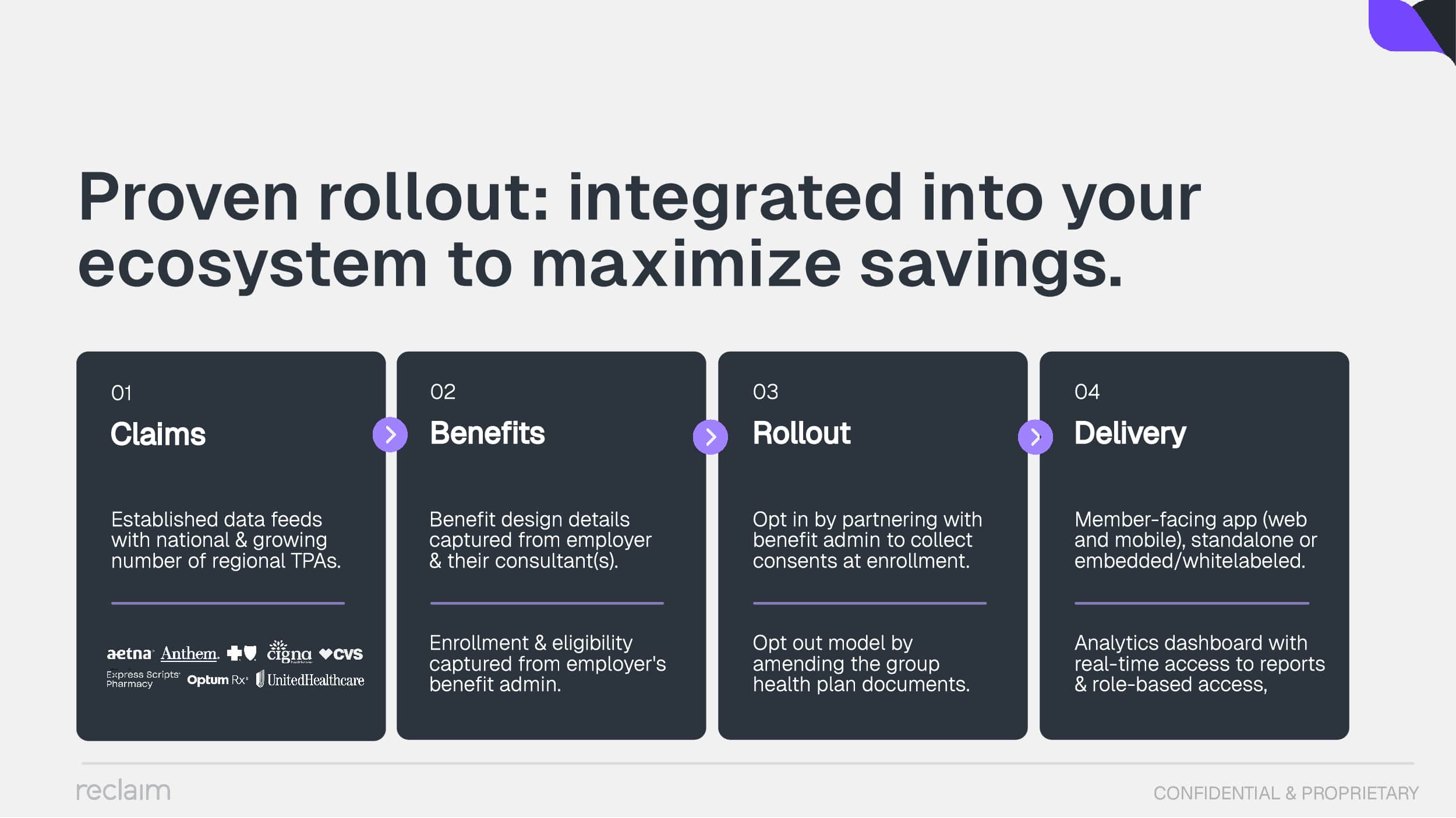
Getting started with Reclaim is easy. Employers can choose to elect participation by collecting employee consents at enrollment, or use an opt-out model by amending group health plan documents. From there, Reclaim integrates into existing data systems through TPAs or employer data warehouses. Once activated, it runs continuously, requiring no ongoing effort from HR or employees.
Reclaim Health is revolutionizing the way healthcare benefits are managed and experienced. Combining artificial intelligence with proactive advocacy and seamless integration helps organizations reclaim millions in lost dollars while supporting employees in navigating healthcare with ease.
For employers looking to optimize their benefits investment and offer meaningful support to their workforce, Reclaim is a transformational partner.
Learn more at reclaimhealth.com
For more information, contact them at:
In case you missed it: Log in to access the full Meet A Vendor Presentation!
Not a subscriber? Request access.
Did you find this article interesting?
Don’t keep this knowledge to yourself – share it on your social media channels and spark engaging conversations!