In This Post:
Presenters:

Sarah Ziemer
Senior Vice President of Employer Sales
According to the CDC, the number of people managing two or more chronic conditions has surged dramatically, with a 142% increase since 2001. What was once an issue primarily for older adults is now accelerating among younger populations as well. More than half of the population is now living with multiple chronic conditions (MCC), and that fact has become impossible to ignore.
This shift has created both a human and financial tipping point. Employers and health plans face unsustainable costs, while individuals struggle to navigate fragmented systems of care that address conditions in isolation rather than the whole person. MOBE is designed to strengthen current health management efforts through tailored content and one-to-one guidance.
In a recent webinar, Sarah Ziemer, Senior Vice President of Employer Sales at MOBE, shared the “missing link” of going beyond traditional, single-condition approaches to uncover the true drivers of cost and care. A cross-condition, whole-person solution that integrates care, optimizes medications, and supports healthier daily habits.
About MOBE
MOBE delivers innovative, effective solutions that support both employers and employees. With their teams, MOBE is making a difference in the health care space, person by person. They leverage claims data to identify long-term, frequent use of healthcare services – based on utilization versus cost/risk/condition.
Engaging and supporting multi-chronic individuals (~20% of a population), who are not yet high-cost claimants, is what MOBE does using a whole-person, cross-condition program blending medication optimization (pharmacists) and lifestyle guidance (health guides) – avg. 30% 1:1 engagement. The entire MOBE program is paid for through generated savings – if there are no generated savings, MOBE’s program is free.
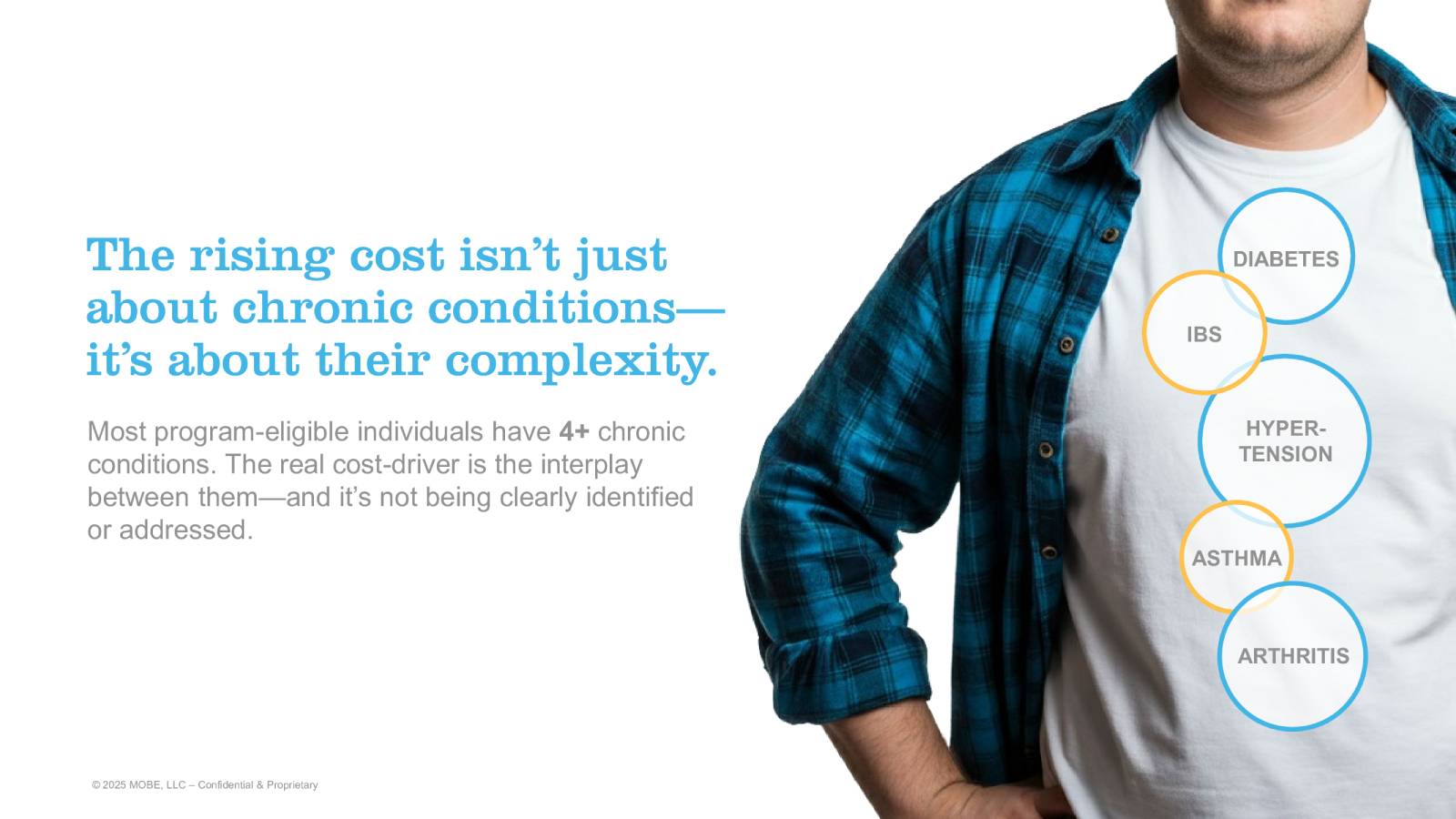
The Complexity Behind Rising Costs
The rise in costs is not simply about the presence of chronic conditions. It’s also about their interplay and complexity. Research shows that most individuals who are program-eligible have four or more chronic conditions, which often overlap in unpredictable and costly ways.
Consider a typical case: a person living with diabetes, hypertension, arthritis, and asthma. The symptoms and treatments for these conditions can overlap, causing side effects such as sleep disruption, increased stress, or worsening mental health. Fragmented care frequently leads to unnecessary medications, duplicate diagnostics, and repeated emergency room visits or hospital stays.
This is why treating each condition in a silo falls short. The real cost driver is how multiple conditions interact with each other and the person’s overall lifestyle.
The Problem with Single-Focus Solutions
The health and wellness market has over 1,200 single-focus solutions, from diabetes management apps to hypertension coaching programs. While many of these tools offer value in isolation, they fail to meet the needs of the growing multi-chronic population.
Key challenges include:
- Condition-specific outreach isn’t relevant to people juggling multiple health concerns.
- Providers’ reimbursement structures are not aligned with whole-person care and often don’t support necessary lifestyle changes.
- Care management programs are forced to focus narrowly on the highest-risk, highest-cost individuals, leaving many without adequate support.
As a result, individuals often bounce between multiple programs, multiple providers, and multiple medications with no clear integration or coordination.
A Whole-Person, Cross-Condition Approach
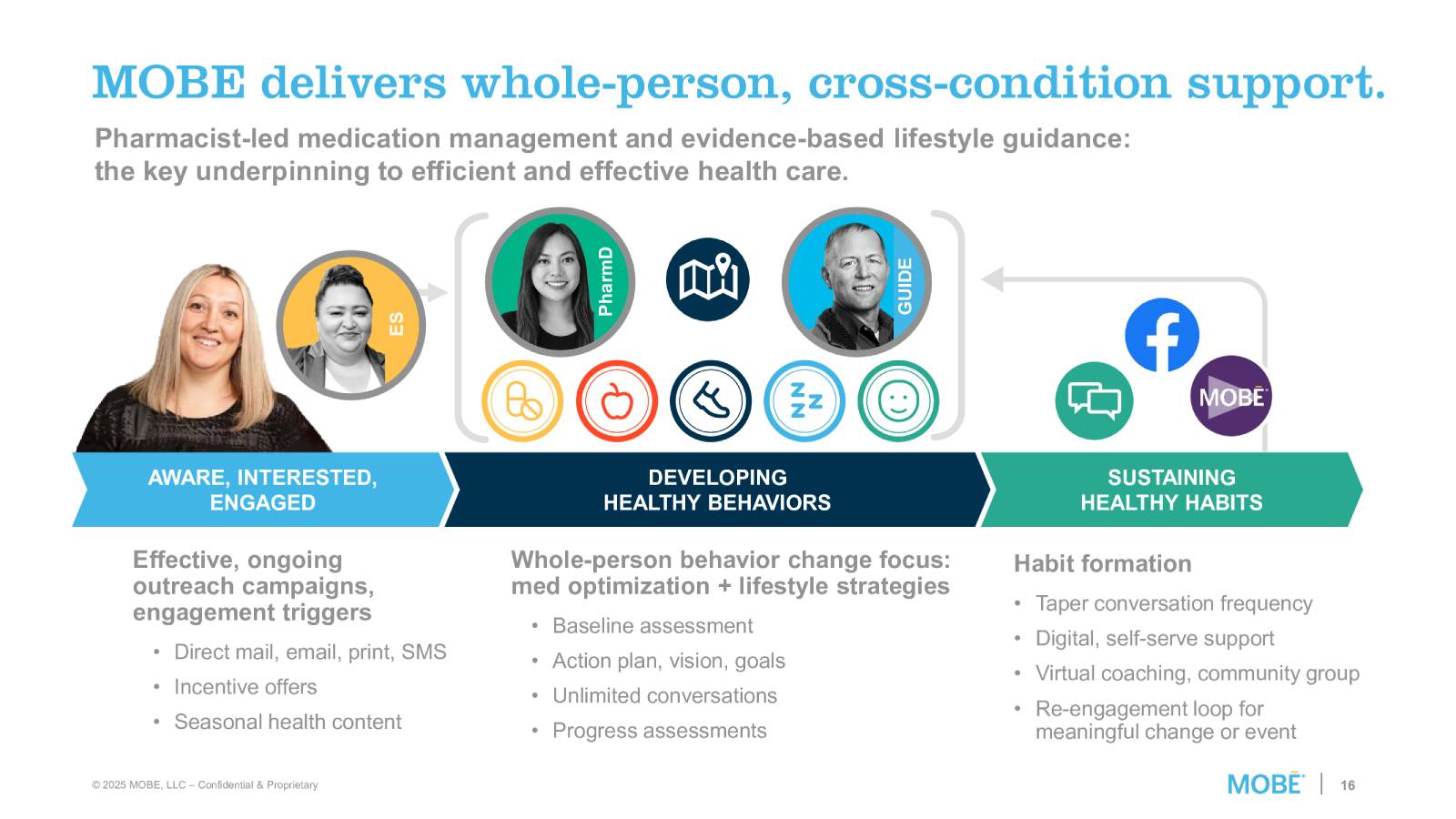
This is where MOBE steps in. By focusing on the whole person, rather than just their conditions, MOBE’s approach bridges the gaps that traditional systems leave behind.
The MOBE360 solution is built on three pillars:
- Population. MOBE identifies individuals not just by diagnoses but also by utilization patterns, risks, and behaviors. About 20% of a covered population typically qualifies those with multiple chronic conditions, rising risks, and a high likelihood of benefit.
- Program. The program combines medication optimization with evidence-based lifestyle strategies, ensuring that people not only take the proper medications in the right way but also build healthier daily habits around nutrition, activity, sleep, and stress management.
- Engagement. Personalized engagement strategies align with individuals’ personal motivations and are supported by unlimited one-on-one conversations, virtual coaching, community groups, and digital tools. MOBE funds and fulfills all outreach and incentives, reducing the administrative burden on employers.
Real-World Results
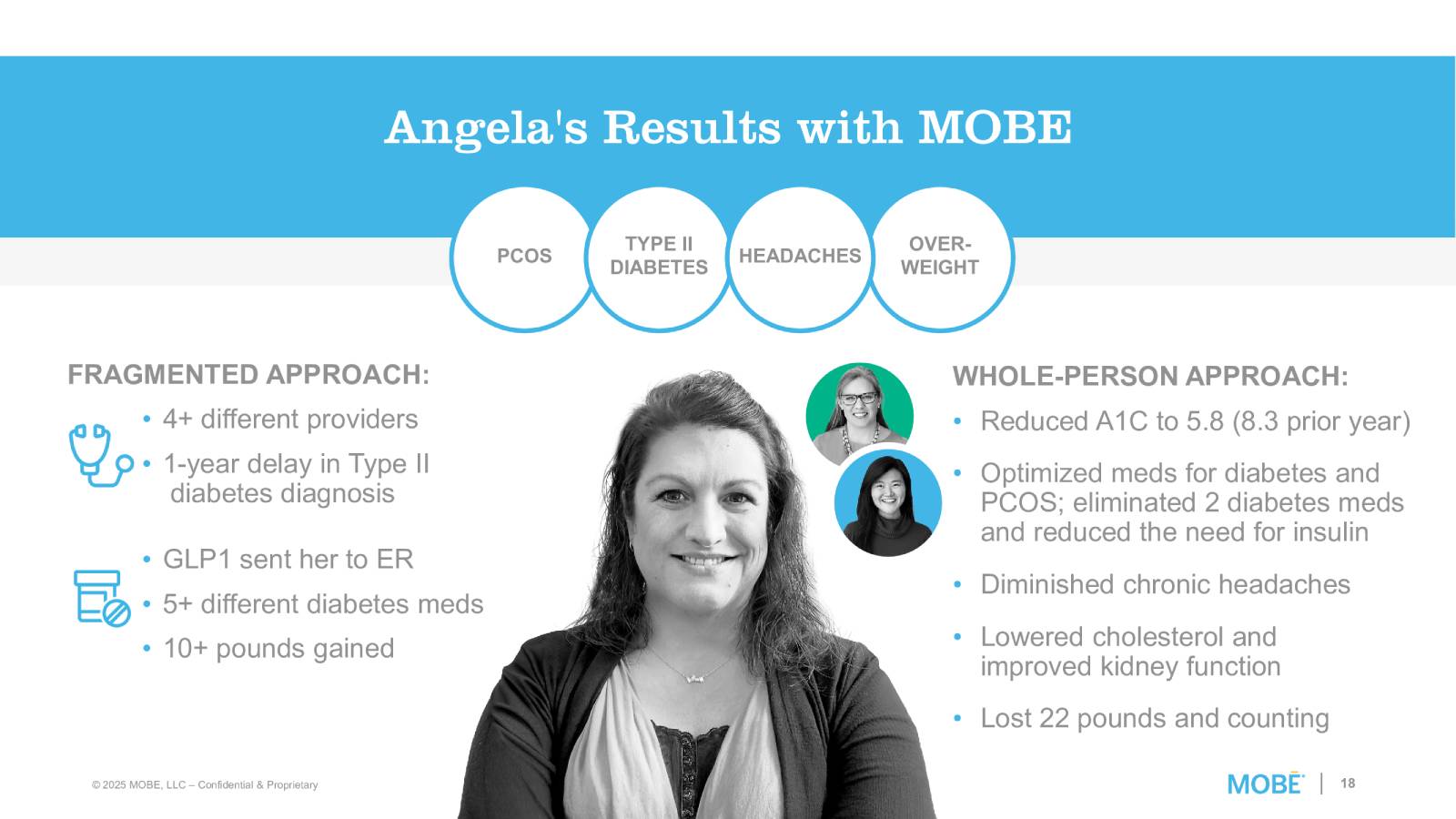
The impact of this approach is best illustrated through participant stories.
Take Angela, for example. Before MOBE, she was navigating PCOS, Type II diabetes, and chronic headaches across multiple providers. She had delayed diagnoses, experienced medication complications, and was gaining weight despite various prescriptions. With MOBE’s whole-person support, Angela reduced her A1C from 8.3 to 5.8, optimized her medications, lost 22 pounds, and improved her kidney function and cholesterol, all while reducing reliance on unnecessary treatments.
Other participants have seen similar results:
- Lauren reduced her medications from 6 down to 2, improved her sleep, and controlled blood pressure.
- Koshie improved sleep by 3 hours per night, lost 19 pounds, and eliminated 10 prescriptions.
- Blake transformed from sedentary and struggling with substance use to running 10 – 15 miles a day, giving up alcohol, and losing 60 pounds.
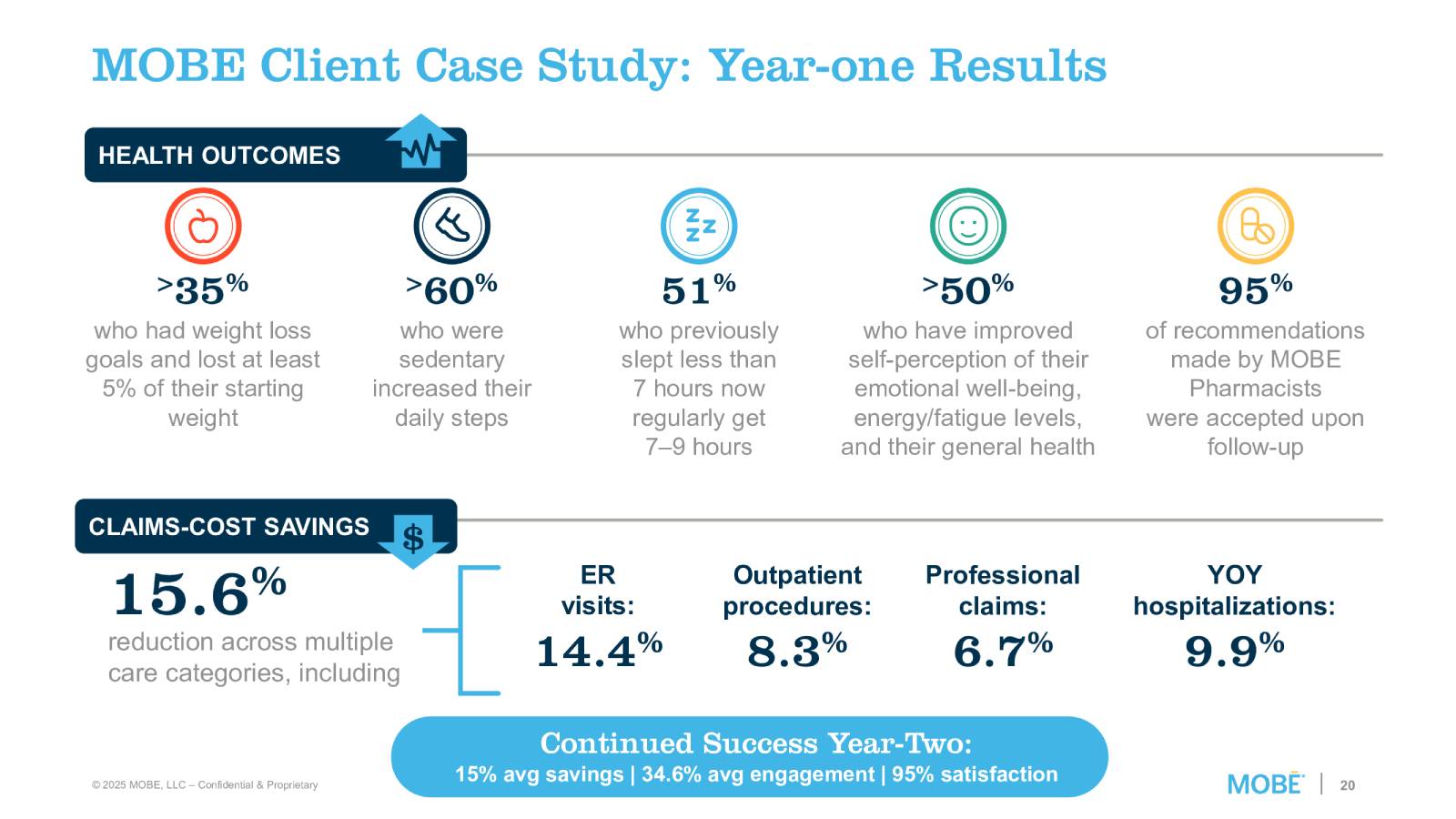
These outcomes are not isolated. Across MOBE participants:
- >35% lost at least 5% of their body weight.
- >60% who were sedentary increased their daily steps.
- 51% improved sleep to a healthy 7 – 9 hours.
- 95% of pharmacist recommendations were accepted by providers.
The Financial Case
Health outcomes are only part of the story. MOBE also delivers measurable savings. Clients see:
- 7.5% average year-one savings
- Reductions across ER visits (15.6%), hospitalizations (6.7%), outpatient procedures (14.4%), and professional claims (8.3%)
- Continued year-two savings averaging 15%, with strong participant satisfaction and engagement rates.
What makes MOBE’s model even more compelling is its 100% fees-at-risk approach. Program costs are tied directly to outcomes such as claims-cost savings, participant engagement, and lifestyle improvements. This guarantees employers a return on investment and aligns MOBE’s incentives with both health and financial outcomes.
Get in touch with MOBE today!
The multi-chronic population is growing rapidly, and traditional single-focus solutions are not enough to meet their needs. To improve quality of life, organizations must embrace whole-person, cross-condition support that integrates medication management with lifestyle coaching and meaningful engagement.
MOBE’s model demonstrates that when you treat the whole person, not just their diagnoses, you can unlock better health, reduce costs, and create sustainable change. For employers, payers, and individuals alike, this approach represents the missing link to both health and savings.
For more information, contact:
Sarah Ziemer – sarah.ziemer@mobeforlife.com
In case you missed it: Log in to access the full Meet A Vendor Presentation!
Not a subscriber? Request access.
Did you find this article interesting?
Don’t keep this knowledge to yourself – share it on your social media channels and spark engaging conversations!