
Doctor on Demand: The Future of Telehealth Services
What does Doctor on Demand cost people with and without insurance coverage, and is it better than in-person appointments?

Chairman at CalltheCare

Owner of Erez Functional Medicine
Obesity Medicine Specialist at Restore Care
The pandemic, and the economic challenges that followed, exposed many inequities in the global healthcare system.
As COVID-19 spread, it became clear that some groups were hit much harder than others, not just because of the virus itself but due to social and economic factors.
It highlighted a more significant issue: many diseases, including diabetes, disproportionately affect specific populations. Data shows that diabetes rates can vary significantly based on factors like income and healthcare access, beyond genetics.
However, there is a silver lining: growing awareness of health equity in the workplace has inspired business leaders to explore how to better address these disparities— primarily through diabetes programs.
This article explores how social determinants of health (SDOH) shape diabetes risks and outcomes in the workplace.
A health crisis in slow motion is how many health professionals describe the toll of diabetes. Though it is a familiar disease that lacks a sense of urgency, it has already surpassed infectious diseases like malaria and HIV in global mortality.
In fact, since 2000, diabetes has risen by 95%, now ranking among the top ten causes of death according to the World Health Organization.
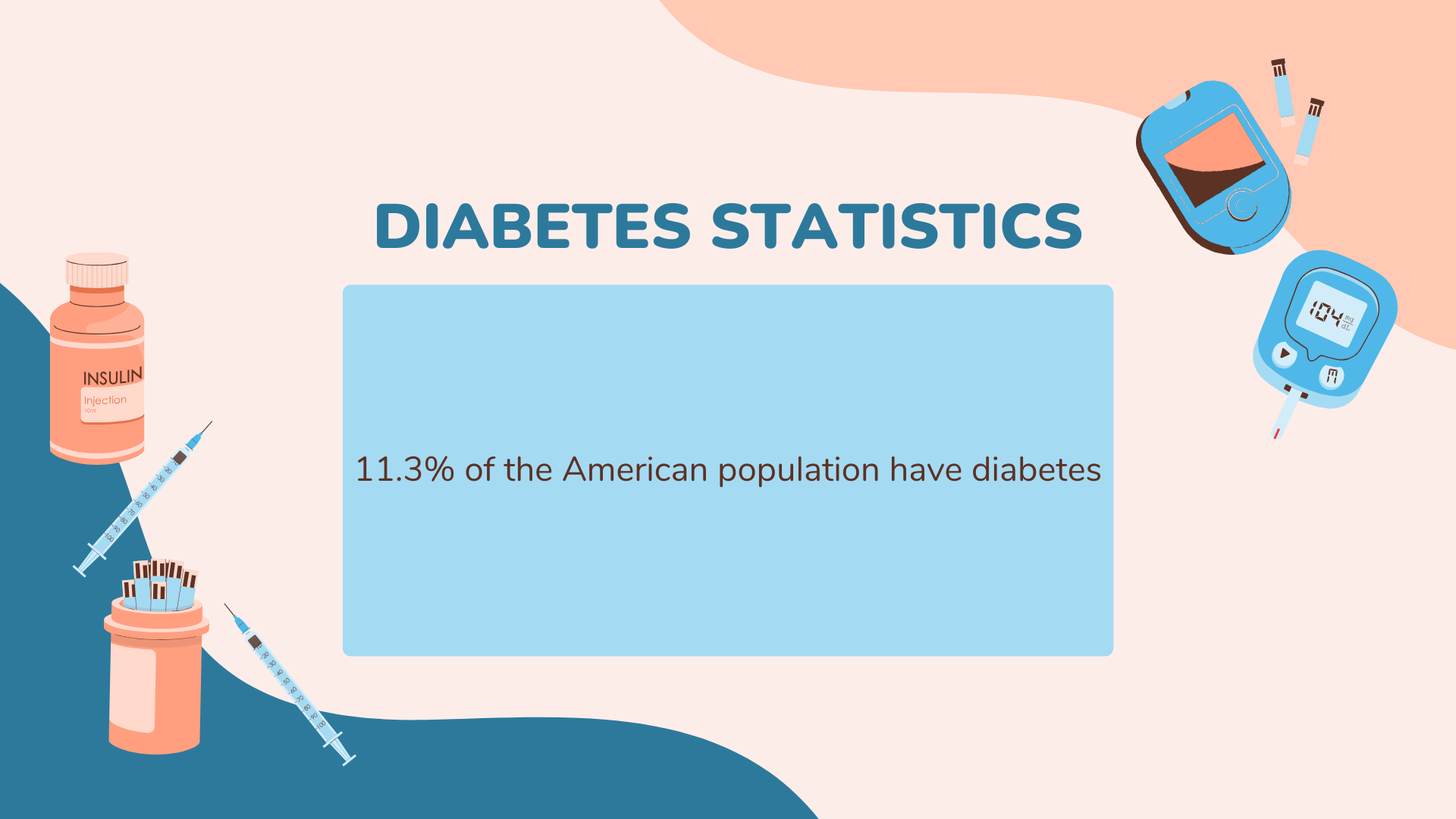
Diabetes statistics show that 11.3% of the American population have diabetes, making it omnipresent in all types of workplaces and industries and affecting employees at every level.
While diabetes today is recognized as a disability under the Americans with Disabilities Act (ADA) with certain protections, much progress still needs to be made.
For example, type 2 diabetes (T2D) is often stigmatized as a result of personal lifestyle choices, ignoring the complex socioeconomic, environmental, and genetic factors involved.
With over 1.3 billion people at risk of developing diabetes, it’s clear that this isn’t a series of personal failures but rather a complex societal challenge.



The good news is that effective treatments for diabetes do exist.
The bad news is that not everyone has equal access to these treatments.
In the United States, persistent disparities affect various racial and ethnic communities in many ways. These inequalities often build on each other, affecting overall health, daily life, and work experiences.
For these reasons, we now recognize that health is personal and often driven by larger systemic causes.
So, to address health equity in the workplace, it’s crucial to understand the social determinants of health (SDOH), which account for 50-60% of health outcomes.
Can our jobs, zip codes, and traditions shape health disparities?
Surprisingly, yes. A wealth of research supports the idea that social and environmental factors can affect diabetes development, treatment, and outcome.
In short, the places where we’re born, live, and work — known as social determinants of health — play a significant role in shaping diabetes risks.
Below, we explore some of the ways that SDOH factors can impact diabetes in the workplace.
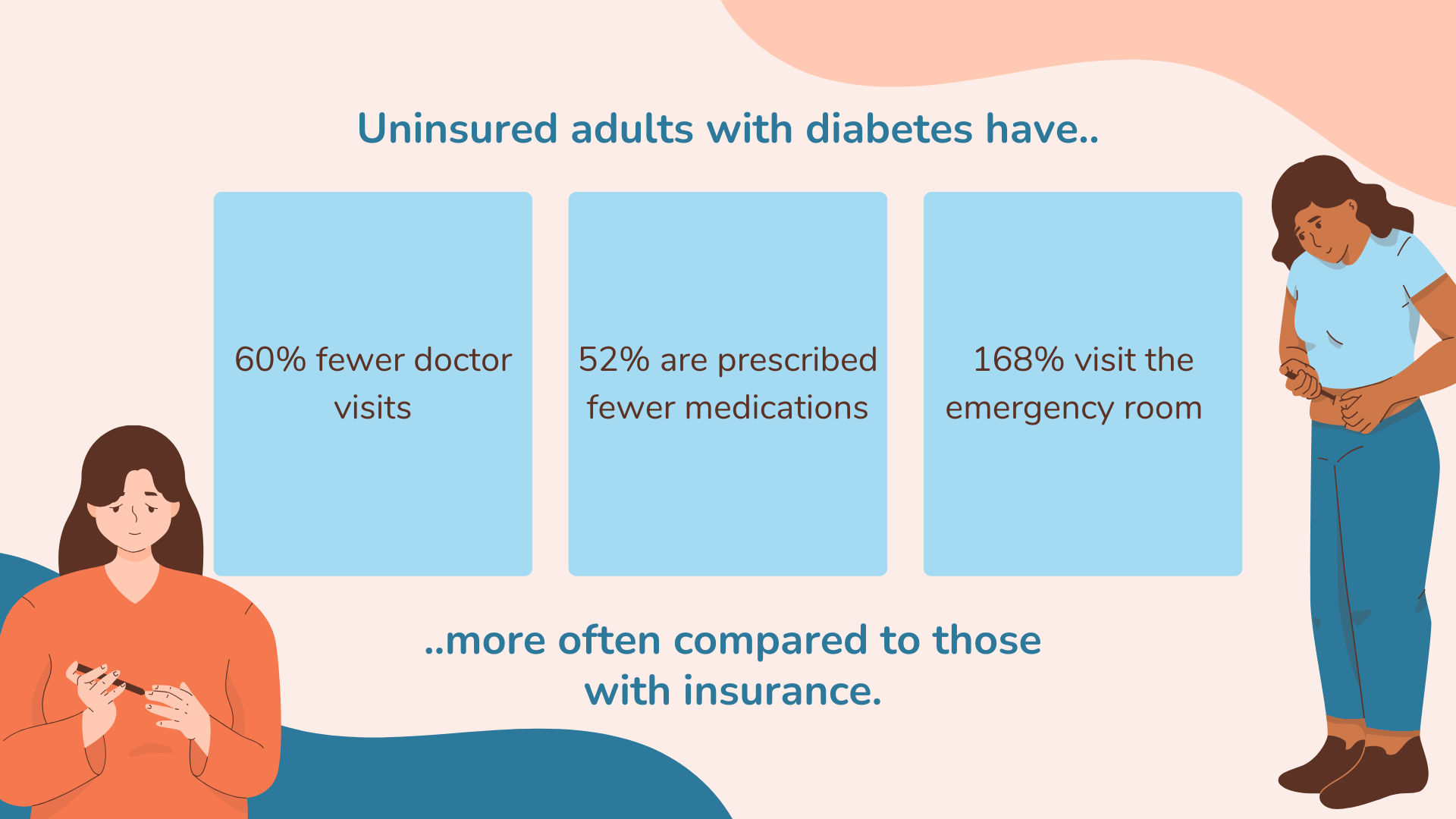
In many studies, getting healthcare insurance is the strongest predictor of whether adults with diabetes have access to diabetes screenings and care.
Uninsured adults with diabetes have 60% fewer doctor visits, are prescribed 52% fewer medications, and visit the emergency room 168% more often compared to those with insurance, according to research.
However, access to health services is more than simply having medical insurance. In fact, many employees with employer-sponsored healthcare coverage still face barriers when accessing healthcare, such as:
On average, healthcare costs for people with diabetes are more than double those without the condition. For these reasons, around 14% to 20% of adults with diabetes say they cut back or delay taking medications because of the expense.
Knowledge is power, and when it comes to diabetes, it can be lifesaving.
Attaining higher education improves health literacy and enables people to understand better, use, and access health resources.
When we examine the data, it’s clear that higher levels of education are linked to lower diabetes incidence, better health literacy, and improved access to healthcare resources.
In the U.S., adults with less than a high school education have the highest rates of diabetes (10.4 per 1,000) compared to those with more education, and they also face higher mortality rates—those with a college degree or higher experience the lowest odds of diabetes and related deaths.
Cultural and social factors also play a great role in shaping health outcomes, particularly in the context of type 2 diabetes.
Strong connections to culture, family, and community can improve health. On the other hand, studies have shown that a lack of social cohesion and experiences of racism and discrimination can contribute to higher diabetes rates, especially among marginalized communities.
For example, the Black Women’s Health study found that women with the highest exposure to everyday racism had a 31% increased risk of diabetes.
Furthermore, social factors like family obligations, traditional gender roles, and unhealthy food customs can act as barriers to healthy living.
As a person’s income decreases, the risk of developing diabetes rises drastically.
When money is tight, employees struggle to afford health resources like nutritious food, medical care, and exercise.
So, how wide is the health gap between financially secure employees and those struggling to make ends meet?
Compared to high-income workers, middle-income employees face a 40% higher prevalence of diabetes, those near poverty see a 74.1% increase, and those in poverty experience more than double the rate.
In fact, research highlights that income and health are linked at every economic level, with a clear gradient: middle-class Americans are healthier than those near poverty, but they are still less healthy than the upper class.
Urbanization has been the greatest demographic shift of the past century, forever changing our neighborhoods and built environments.
Our environment determines exposure to factors such as pollution, the availability of grocery stores, and walkable spaces—all of which influence stress levels and the risk of developing diabetes.
So, does our zip code really affect the likelihood of developing diabetes?
Studies, such as those from The Lancet, show that living in a “food swamp”—where fast food and junk food outnumber healthier options—is directly linked to a higher prevalence of type 2 diabetes.
Access to local resources—such as green spaces, recreational areas, and reliable transportation—also impacts health.
In addition, research has connected air pollution to increased diabetes risk by triggering inflammation and altering the microbiome.

Managing diabetes at work can be a daily struggle. Unlike other chronic illnesses in the workplace, diabetes requires constant attention.
According to the CDC (Centers for Disease Control and Prevention), just 45% of people with type 2 diabetes and 25% of those with type 1 diabetes can reach their target blood sugar levels.
Employees with diabetes need to regularly check their blood sugar, make careful meal choices, and often take insulin multiple times a day.
But how do the social determinants of health (SDOH) play into this?
Things like income, education, and access to healthcare can make managing diabetes at work easier—or much more complicated.
For example, lower-income employees may struggle to afford insulin or healthy food. They might not have access to a refrigerator at work or home to store their insulin safely.
Workers in rural areas could face long drives to their doctors, making it tough to get timely care.
And those working high-stress jobs or irregular shifts may find it difficult to keep their blood sugar levels stable due to inconsistent meals or poor sleep.
So, what can workplaces do to help?
Diabetes is a major driver of healthcare costs, with 36% of large employers ranking it among their top three cost concerns.
Since diabetes and prediabetes affect so many workers, it’s beneficial for employers to find ways to support them, lower costs, and improve health equity in the workplace.
To promote health equity, employers must design wellness programs that are culturally inclusive and tailored to the needs of diverse populations.
According to Armen Gazaryan, Chairman of CalltheCare, “Employers can promote health equity for employees with diabetes by providing them with comprehensive wellness programs, including regular health screenings, diabetes education, and the option to consult healthcare professionals.”
He emphasizes that creating an open environment where employees feel safe discussing their health without fear of stigma is key.
Workplaces can also implement simple initiatives, such as providing healthier food options in cafeterias, organizing regular physical activity sessions, and ensuring that health insurance covers diabetes management.
“Policies and programs should be devised on the rubric of being inclusive and supportive to workers suffering from diabetes,“ adds Gazaryan.



November being National Diabetes Awareness Month offers a perfect time for employers to strengthen their diabetes-related support.
John Lowe, Obesity Medicine Specialist at Restore Care, stresses the need for comprehensive health coverage, explaining that “Health insurance plans should be provided by employers that cover diabetes management, such as medicines, glucometers, and referrals to experts.
Additionally, mental health services should be covered because managing a chronic condition like diabetes can affect one’s state of mind.”
Dr. Aaron Erez, owner of Erez Functional Medicine, emphasizes the importance of flexibility, noting, “Flexible work options are key. Many of my patients struggle when rigid work schedules conflict with the demands of managing diabetes.”
He adds that offering telecommuting, flextime, or part-time schedules can allow employees to stay healthy while remaining productive.
Dr. Erez also highlights the value of small accommodations, stating, “Things like access to a refrigerator for insulin, breaks to check blood sugar or eat snacks, and a private space for injections or pumps are simple but meaningful.“
Employers can play a vital role in promoting health equity by partnering with community-based organizations (CBOs), faith-based organizations (FBOs), and community health workers (CHWs) to help manage and prevent diabetes.
CBOs, in particular, are well-positioned to tailor diabetes programs because of their deep connections within local communities.
Their understanding of the cultural, social, and economic factors unique to the populations they serve allows them to adjust programs effectively to meet local needs.
From local charitable foundations to YMCAs and churches, these groups are trusted by the community and often have experience addressing health-related social needs, making them valuable partners in delivering impactful health interventions.
Employers can also fund local educational programs and back efforts like increasing access to fresh produce at farmers’ markets, launching outdoor walking groups, and offering incentives for regular health screenings.
In 2022, NEBGH shared a guide titled Obesity, Diabetes and Racial Health Equity: What Employers Can Do, offering strategies for HR and benefits leaders to address health disparities in diabetes and obesity care.
The guide recommends actions employers can take, such as:
Evaluating healthcare vendors on their DE&I practices, including the diversity of provider networks
Technology has become an integral part of our lives and, by extension, our health.
Today, many employers offer digital platforms to help employees and their dependents reverse prediabetes and diabetes.
Unlike traditional weight loss programs, which tend to focus more on general strategies, these digital platforms take unique approaches to engaging employees.
For example, some use tools like wireless scales and mobile apps to send personalized reminders for healthy eating and physical activity while connecting employees to healthcare providers, coaches, and community resources.
Others combine nutritional counseling with telehealth coaching and remote monitoring. In a two-year study using such a combination, 97% of prediabetic participants avoided progressing to type 2 diabetes, saving employers an estimated $381 per patient per month.
Other platforms focus on medication-assisted therapies, such as GLP-1 drugs like Ozempic, which have shown a 15% average weight loss and an 84% improvement in A1C levels.
These digital solutions offer a range of options to meet employees’ diverse needs and address health equity in the workplace.
The future of health equity in the workplace depends on creating environments where all employees can thrive. To achieve that, employers can take action in three simple areas:
These efforts not only help prevent and manage conditions like diabetes but also contribute to a healthier, more equitable workforce overall.
Disclosure: Some of the products featured in this blog post may come from our partners who compensate us. This might influence the selection of products we feature and their placement and presentation on the page. However, it does not impact our evaluations; our opinions are our own. The information provided in this post is for general informational purposes only.
Senior Content Writer at Shortlister
Browse our curated list of vendors to find the best solution for your needs.
Subscribe to our newsletter for the latest trends, expert tips, and workplace insights!

What does Doctor on Demand cost people with and without insurance coverage, and is it better than in-person appointments?

Are you doing enough to support employees with chronic conditions, or are rising healthcare costs and absenteeism quietly impacting your bottom line?

Can fertility benefits become a recruiting and retention magnet in the ever-evolving workplace landscape?
Beyond legal compliance, accommodating chronic illness in the workplace has become a strategic tool for companies to control costs and improve employee well-being.
Used by most of the top employee benefits consultants in the US, Shortlister is where you can find, research and select HR and benefits vendors for your clients.
Shortlister helps you reach your ideal prospects. Claim your free account to control your message and receive employer, consultant and health plan leads.