
2025 is About The Great Detachment
In 2025, employee detachment is quietly draining workplace energy. Explore how leaders can step in to re-engage their teams, reignite motivation, and rebuild a sense of purpose.


CEO & Founder of Ambari Nutrition
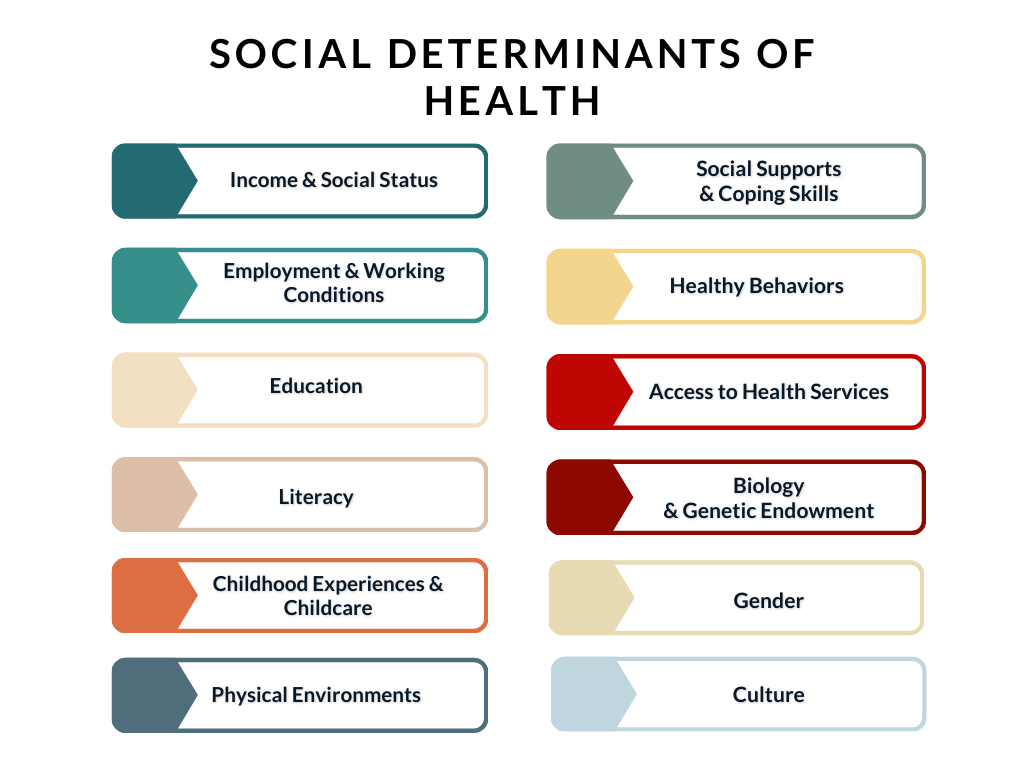
Until recently, social determinants of health (SDoH) were only linked with participants in public healthcare insurance programs like Medicare and Medicaid, or those without healthcare coverage.
However, as the COVID-19 pandemic brought to light many healthcare disparities and their causes, more employers have started to focus on tracking and addressing these factors.
So, what are the social determinants of health?
Research gathered from the last few decades has found that the conditions and circumstances in which people live, and work have a powerful effect on their health and longevity.
In other words, people disadvantaged by socioeconomic circumstances and neighborhood environments – such as poor education and housing, insecure employment, and low income – have worse health from birth throughout life.
Despite substantial efforts dedicated to improving access to high-quality healthcare, the United States continues to experience disparities in health outcomes based on factors like race, ethnicity, sexual orientation, gender identity, and disability, and economic and community factors such as geographic location, income level, and employment status.
In this article, we explore these non-medical factors that are well-understood as social determinants of health and their complex relationship with health outcomes.
Most of us have noticed a direct link between our income, social status, and health in our lives. Namely, regular income and the amount earned dictate how much we spend on essentials like housing, food, and health care.
Health and wealth are closely related, and a large body of research has established their interconnectedness. Compared to higher-earning adults, those with lower incomes have higher rates of chronic diseases, such as diabetes, heart disease, stroke, and lower longevity.
However, health disparities linked to income begin at a much younger age than is commonly known.
As evidenced by research, low-income mothers have the highest rates of low birthweights, while lower-income children have higher rates of health problems like asthma and heart conditions.
Unfortunately, in the United States, one in ten people live in poverty and can’t afford even essentials like housing and health care. One significant way that income influences health outcomes is that people with lower incomes experience greater barriers to accessing health care.
Employers can help mediate the adverse effects of income and social status on health by providing a livable wage and robust health and wellness benefits.
Shortlister’s article “How to be Happy at Work” discusses how employees can find long-lasting fulfillment and whether being jobless will make people happy.
However, as the article points out, unemployment is bad for our mental and physical health, as it leads to a loss of social connectedness, lack of daily structure, and, perhaps the most impactful factor to our health – loss of societal status and income.
Lack of employment is associated with many behavioral and mental health problems, such as stress, depression, and anxiety.
For most Americans, employment provides economic stability and lifts people out of poverty. However, being employed does not necessarily guarantee a decent living.
Despite being employed, eight percent of the global workforce lives in conditions of extreme poverty.
Multiple aspects of employment – including the work environment, job stability, financial compensation, and physical safety – may affect health.
The nature of work, such as a stressful job with poor work-life balance, a toxic work environment, or a job that doesn’t adhere to OSHA regulations of workplace safety, increases the risk of negative health outcomes.
Since Americans spend half their waking hours at work, employment, along with factors like poverty and education, have the largest impact on health outcomes.
Generally, being well-educated is equated to a higher income, better job, greater literacy, and a greater understanding of the consequences of unhealthy behaviors – all of which lead to better health.
Research also consistently indicates a direct correlation between higher educational attainment and improved health and well-being.
College graduates generally report better health compared to those with only a high school education, and people with more education are less likely to suffer from various health conditions like heart disease, hypertension, diabetes, anxiety, and depression.
Individuals with lower education often have fewer job choices, potentially leading to roles with limited authority, job insecurity, and lower pay. They are also more likely to engage in physically demanding work or work involving exposure to harmful substances.
Furthermore, in the United States, limited English proficiency can limit access to healthcare services and the understanding of health information. Those with limited English skills are often less likely to have a regular healthcare provider or to receive preventive care.
Research focusing on Hispanic adults in the US revealed that those responding to a health survey in Spanish reported poorer health status compared to those responding in English, irrespective of their specific Hispanic origin.
Continuous learning and development, career training, and student loan assistance can all encourage employees to create a culture of lifelong learning that benefits all.
The first five years of a child’s life play a critical role in shaping their long-term social, cognitive, emotional, and physical development.
When children are exposed to early life stressors such as physical abuse, family instability, unsafe neighborhoods, or poverty, they can develop inadequate coping skills, struggle to regulate their emotions, and have impaired social functioning compared to other children their age.
Perhaps the most critical factors in early childhood development are:
High-quality childcare is vital as it means children can have improved nutrition, better access to health screenings, and improved mental health later in life.
But today, affordability, access, and conflicting schedules remain barriers for many, especially low-income families. In 2019, family support services, including childcare, were the social services most in demand by healthcare consumers.
In the United States, three in four working parents reported their job has been affected because of issues with childcare, and within the last year, one in three employees missed work due to childcare issues.
Similarly, childcare benefits have been identified by Shortlister in the “Workplace Wellness Trends Report for 2024” as the benefit experiencing the highest year-on-year increase in demand.

From our quality of housing to basic amenities and the levels of crime and violence in our neighborhoods – our physical environment plays a role in our health outcomes and life expectancy.
In fact, up to 60% of our health is determined by our zip code, far more than our genetic codes (30%).
One of the biggest factors affecting health outcomes is housing instability: when your primary concern is your family having a roof over their heads, doctor’s appointments can no longer be a priority.
But affordable housing is becoming less attainable in America.
A quarter of owner households and nearly half of renter households are cost-burdened, meaning that people pay more than 30% of their income for housing.
As a result, many Americans may have difficulty paying for food, transportation, clothing, and medical care after covering their rent and mortgage payments.
Many people resort to living in substandard housing conditions, which can open up a host of other health issues, such as lead exposure, poor ventilation, mold, overcrowding, pest infestation, and other health hazards.
Furthermore, the wider environment can play a role in our health. Kevin Huffman, CEO & Founder of Ambari Nutrition, shares, “Environmental factors—air and water quality—affect our health profoundly; poor conditions often yield a surge in respiratory diseases, cancers, and chronic ailments—all exacerbating the plights of vulnerable groups.”

Social well-being is a usually overlooked wellness dimension that influences health and overall quality of life. People thrive when they develop a sense of belonging and establish strong community connections.
Relationships, social cohesion, and interpersonal bonds are essential for physical health and psychological well-being. In simpler terms, being kind to your neighbor and volunteering in your local community is beneficial for your health.
However, many people in America are experiencing a loneliness epidemic.
Loneliness and social isolation affect everyone, from younger generations to single parents with children, the elderly, and even underrepresented members of the community.
Unsurprisingly, high levels of support from friends, family, and communities are associated with better health outcomes. When people live in stable, diverse, cohesive, and safe communities, their overall health is enhanced.
On the other hand, stressful experiences that are related to discrimination can worsen people’s health. Discrimination, especially racial discrimination, can lead to symptoms of trauma.
Companies must prioritize diversity, inclusivity, and equality (DEI) in their workplace and provide access to employee assistance programs (EAPs), which can help teach employees coping skills for struggling employees.
While it’s true that our choices significantly impact our health, framing healthy behaviors solely as individual decisions ignores the crucial role of social determinants in shaping those choices.
Just as access to education, income, and housing varies vastly across populations, so too does access to the resources needed to pursue healthy habits.
While smoking, diet, substance abuse, and exercise are often individual choices, the ability to make these choices freely is heavily influenced by external factors.
Low income might restrict healthy food options, lack of green spaces limit exercise opportunities, and inadequate education leave one more vulnerable to misinformation about health risks.
Other examples are neighborhoods with limited physical access to affordable and nutritious food, also known as food deserts, and residential areas with a high density of fast food and junk food, called food swamps, which influence dietary choices and employee health.
According to research, living in a food desert is linked to a greater risk of obesity and a poor diet.
So, by acknowledging the complex relationship between social determinants and healthy behaviors, we can move beyond a simplistic “individual responsibility” model and tackle structural barriers that prevent people from making healthier choices.
The ease of accessing high-quality healthcare services and understanding when and how to seek care can greatly determine health outcomes.
Kevin Huffman comments, “As a doctor of osteopathic medicine, I understand that elements such as income level, education status; employment situation; strength of social support networks; and availability—and affordability—of medical services aren’t mere abstract ideas.
Instead, these variables tangibly determine whether someone can secure appropriate care—and indeed if they can benefit from it at all.
An individual residing in a socioeconomically deprived area often faces challenges: struggling to access high-quality health facilities and affording necessary treatments; these barriers invariably result in poorer health outcomes. It is our duty, then—to consider and address meticulously these social determinants—that shape the very fabric of our patients’ lives.”
Statistics show that about one in ten people in the United States don’t have health insurance, meaning that many people in the United States don’t have access to the health care services they need.
On top of that, people often forgo recommended healthcare services like cancer screenings and treatments because of barriers like high cost of care, inconvenient transportation, and inadequate health insurance.
Employers that want to promote health, prevent diseases, reduce healthcare costs, and achieve health equity must reevaluate their healthcare plans through an equality lens.

Our genetic makeup plays a significant role in shaping our health.
Specific genes can increase or decrease an individual’s risk of developing particular diseases.
For example, the BRCA1 and BRCA2 genes are linked to an increased risk of breast cancer, while the APOE-e4 gene is associated with a higher risk of developing Alzheimer’s disease.
However, it’s important to remember that genes are not destiny.
While they may provide a blueprint, environmental factors, and lifestyle choices significantly influence how those genes are expressed.
A healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, can mitigate the negative effects of certain genetic predispositions.
Understanding the complex relationship between biology, genetics, and other factors is crucial for promoting health equity and ensuring everyone has the opportunity to achieve optimal well-being.
In addition, when we understand our biological predispositions, we can make informed choices about our health and take proactive steps to mitigate potential risks.
When discussing health inequalities, we must also mention gender as an essential factor in health outcomes.
Gender is a source of many disparities.
Society treats men and women differently in their workplaces, in their homes, and even in healthcare facilities. Men and women may face different expectations, access to resources, and even the quality of care they receive.
Women may face greater pressure to conform to societal expectations surrounding family roles and domestic responsibilities, which can lead to increased stress and limited opportunities for self-care.
Typically, men work longer work hours, have higher-status roles, and have more physically demanding jobs.
Women, on the other hand, report more mental and physical problems related to work. Women are also paid less for the same amount of work and are more likely to experience sexual harassment and related alcohol abuse.
Even healthcare systems, which strive to provide equal care, can perpetuate inequalities through unconscious biases and gender-based assumptions about health needs.
Recognizing these harmful biases and actively working to dismantle them in healthcare, workplaces, and our everyday lives is crucial to ensuring equitable health outcomes for all genders.
Culture is not just about colorful garments and festive celebrations; it’s a deep-rooted influence shaping our health from the inside out.
From the food we eat to how we approach healthcare, cultural norms, and beliefs can significantly impact our well-being.
Kevin Huffman shares, “Societal influences, such as culture, significantly impact individual health outcomes; they can mold attitudes and behaviors toward health—positively or negatively. The foods we eat, the activities in which we partake, and our approach to seeking medical attention—all reflect deeply ingrained cultural norms.”
Huffman adds, “As doctors witnessing societal norms and environmental stressors, we directly observe their contributions to disease burdens. Treating the illness involves more than medical intervention; it demands advocating for societal changes—changes that pave the way toward healthier communities.”
The problem is that current workplace wellness programs and medical benefits, while valuable, often miss the mark if they ignore SDoH.
Imagine offering gym memberships to employees struggling with food insecurity. The solution lies in recognizing the systemic barriers that can limit the effectiveness of traditional interventions.
While many companies embrace corporate social responsibility initiatives, only some recognize the untapped potential of addressing SDoH within their own workforce. Shockingly, according to some estimates, social determinants of health influence up to 80% of health outcomes.
Therefore, employers have a unique opportunity to stand out by connecting their social impact efforts with the well-being of their employees.
Specifically, employees want assistance with health care costs, housing, transportation, student loan debt, childcare, and access to earned wages before payday.
Addressing these social needs can, in turn, reduce absenteeism, increase engagement, and positively impact business performance, as shown in a 2018 study.
To summarize, SDoH can have either positive or negative effects in the workplace: it’s up to employers how they approach and address them that determines the outcome.
Senior Content Writer at Shortlister
Browse our curated list of vendors to find the best solution for your needs.
Subscribe to our newsletter for the latest trends, expert tips, and workplace insights!

In 2025, employee detachment is quietly draining workplace energy. Explore how leaders can step in to re-engage their teams, reignite motivation, and rebuild a sense of purpose.

What happens when salary ranges go public? Discover how transparency laws are changing the workplace in 2025 – and what’s next.

A degree is no longer the only path to landing a great job. As companies relax their degree requirements, our skills-first hiring guide explores how to redefine employment criteria to build a more diverse and capable team.

Is transformational leadership a viable solution for companies experiencing low employee trust and engagement? Learn as we unpack all elements of this leadership approach.
Used by most of the top employee benefits consultants in the US, Shortlister is where you can find, research and select HR and benefits vendors for your clients.
Shortlister helps you reach your ideal prospects. Claim your free account to control your message and receive employer, consultant and health plan leads.